
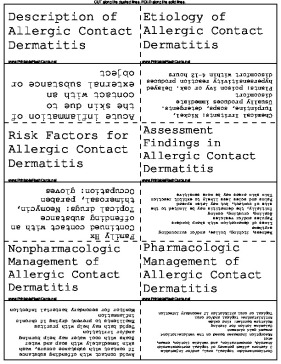
Dermatologists can use these printable skin condition flash cards to study allergic contact dermatitis.
There are 17 flash cards in this set (3 pages to print.)
To use:
1. Print out the cards.
2. Cut along the dashed lines.
3. Fold along the solid lines.
Sample flash cards in this set:




| Questions | Answers |
|---|---|
| Description of Allergic Contact Dermatitis | Acute inflammation of the skin due to contact with an external substance or object |
| Etiology of Allergic Contact Dermatitis | Chemical Irritants: Nickel, Turpintine, soaps, detergents. Usually produces immediate discomfort Plants: poison ivy or oak. Delayed hypersensitivity reaction produces discomfort within 4-12 hours |
| Risk Factors for Allergic Contact Dermatitis | Family Hx Continued contact with an offending substance Topical drugs: Neomycin, thimerosal, paraben Occupation: gloves |
| Assessment Findings in Allergic Contact Dermatitis | Redness, itching, bullae, and/or surrounding erythema Lines of demarcation with sharp borders Papules and/or vesicles Scaling, crusting, oozing Initially, the dermatitis may be limited to the site of contact, but may later spread Palms and soles less likely to exhibit reaction Thin skin areas may be more sensitive |
| Nonpharmacologic Management of Allergic Contact Dermatitis | Avoid contact with offending substance If contact with substance occurs, wash skin immediately with soap and water Soaks with cool water may help burning and/or irritation Tepid bath may help with pruritus Emollients to prevent drying if chronic inflammation Monitor for secondary bacterial infection |
| Pharmacologic Management of Allergic Contact Dermatitis | Corticosteroids: topical, oral, and/or injectable 3 factors affect potency of topical cortocosteroid: Steroid, concentration, and vehicle (lotion, cream, etc) Absorption increases based on the vehicle:Lotion< cream< gel< ointment Calamine lotion for itching Moisture barrier: zinc oxide Antihistamine: topical and/or oral Topical or oral antibiotics if secondary infection |
| Topical Corticosteroids for Allergic Contact Dermatitis | Exert anti-inflammatory effect nonspecifically thru mechanical, chemical, and immunologic means Use lowest potency cream that produces desired effect Skin atrophy is common with long-term steroid use Areas most susceptible are the face, groin, and axillae Topical steroids will worsen skin infections Systemic absorption is usually minimal, but broken skin will absorb significantly more steroid |
| Description of Atopic Dermatitis (Eczema) | Chronic, pruritic skin eruption with acute exacerbations appearing in characteristic sites. Eczema is often used interchangeably with atopic dermatitis, but the word eczema describes acute symptoms associated with atopic dermatitis Commonly seen in pts with other atopic illnesses (asthma, allergic rhinitis) |
| Risk Factors for Atopic Dermatitis | Family hx of atopic dermatitis Skin infections Stress Temperature extremes Contact with irritating substances |
| General Assessment Findings in Eczema | Pruritis Erythema Dry Skin Facial erythema Infraorbital folds (Dennie Morgan folds) |
| Assessment Findings in Infants with Eczema | Lesions on extensor surfaces of arms and legs, cheeks Lesions are erythematous and papular Vesicles may ooze, form crusts |
| Assessment Findings in Children with Eczema | Lesions common in wrists, ankles, and flexural surfaces PResence of scales and plaques; lichenification occurs from scratching |
| Assessment Findings in Adults with Eczema | Flexural surfaces are common sites, dorsa of the hands and feet Often reappears in adulthood after absence since childhood Lichenification and scaling are typical |
| Nonpharmacologic Management of Eczema | Limit bathing (Do not use hot water) to avoid further drying of skin Prevent skin trauma (sunburns, etc) Soak for 20 minutes in warm water before applying emollient Wet compresses (Burrows solution) if lesions are weeping or oozing Pt education |
| Pharmacologic Management of Eczema | Topical corticosteroids are the mainstay therapy (Use lowest potency which controls symptoms) Topical immune modulators; Elidel, Protopic Antihistamines (oral and topical) for itching Emollients 2-3 times per day or as needed to correct dry skin Oral corticosteroids may be used for severe disease, this should be reserved and only used in short bursts Intralesional steroid injections |
| Topical Immune Modulators Used in Atopic Dermatitis (Eczema) | Tacrolimus, Pimecrolimus Potent immune modulators which inhibit T-lymphocyte activation Do NOT use on infected skin Infection will significantly worsen eczema Potential for systemic absorption may increase formation of tumors |
| Consultation/ Referral for Eczema | Dermatologist for severe cases or those not responding to treatment |